Intro
Tears have fascinated humanity since antiquity. They have been addressed in poetry, literature and religious writings, paintings, music and cinema.
There are three basic types of tears:
Basal production that lubricates the eye conjunctiva and is part of our immune barriers
Reflex tears for flushing out external irritants
Emotional tears
Anatomy
The lacrimal gland lies at upper external corner of the orbit, responsible for 90% of tear secretion. The remaining 10% is produced by accessory glands placed in the eyelids. Tears leave the conjunctival surface through two holes, the lacrimal punctum.
These holes drain to a lacrimal sac and then to a duct by which the fluid is conveyed into the cavity of the nose. There are a few valves along this pathway to avoid fluid reflux back to the eye.
An excess of tears, during reflex or emotional tears, causes the nose to run, and when exceeding the lachrymal draining capacity, tears will fall from the eyelid onto the cheek. The medical term for this tearing overflow is epiphora.
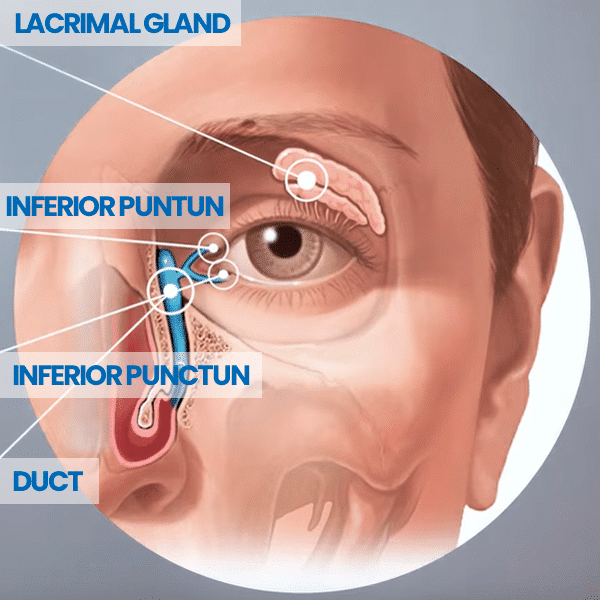
The lacrimal gland lies at upper external corner of the orbit, responsible for 90% of tear secretion. The remaining 10% is produced by accessory glands placed in the eyelids. Tears leave the conjunctival surface through two holes, the lacrimal punctum.
These holes drain to a lacrimal sac and then to a duct by which the fluid is conveyed into the cavity of the nose. There are a few valves along this pathway to avoid fluid reflux back to the eye.
An excess of tears, during reflex or emotional tears, causes the nose to run, and when exceeding the lachrymal draining capacity, tears will fall from the eyelid onto the cheek. The medical term for this tearing overflow is epiphora.
Watery eyes
Having watery eyes affects daily activities, such as reading, driving, outdoor walking, watching television or computer work. It may be caused by an excess of basal tear production or their insufficient drainage.
Let me talk about the latter one, because those are the cases I get referred to.
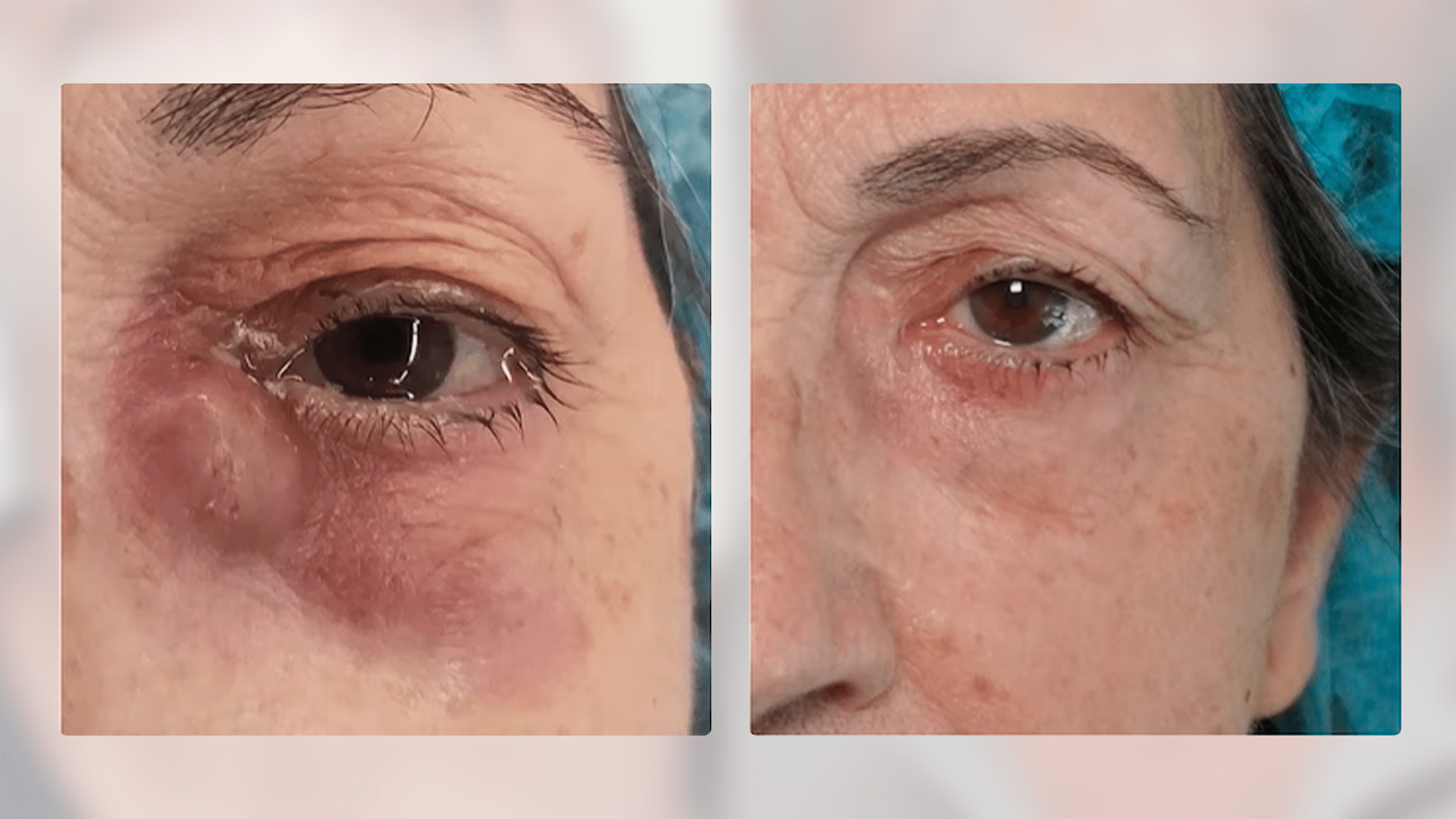
Dacriocystitis
An obstruction in the nasolacrimal system will result in a stagnation of tears and epiphora. Stagnation provides a favorable environment for infectious organisms to propagate and debris to form, leading to a local infection, named dacryocystitis.
There can be obstructions at any level of the nasolacrimal system, for several reasons: local debris, local trauma, lachrymal stones and systemic diseases such as auto-immune diseases.
In adults, dacryocystitis it occurs usually above 40 years old, and females represent around 70% of all cases, because their lacrimal conduit tend to be narrower.
Treatment
During acute infection episodes, it may be necessary to use antibiotic therapy. In chronic dacryocystitis it is almost always managed surgically.
Whatever the case, it is highly recommended to visit an Ophthalmologist before referring to a surgeon.
Surgery is usually performed under general anesthesia, and the approach can be done entirely inside the nose using an endoscope, or combined with a small skin incision. A silicone tube is placed in the lachrymal conduit and left there during a few weeks to prevent re-occlusion.
When for some reason, it is not possible to restore the duct, due to trauma, oncological cases or very fibrotic ducts, a new channel can be opened in the inner corner of the eye with a Jones tube.
Patients leave hospital the same or the next day and should avoid strenuous activities, to prevent unnecessary nose bleeding.
For patients unfit for general anesthesia, there are other possible surgical approaches and managements.

Orbital tumors
Many tumours and pseudotumors (inflammatory disorders) can affect the orbit. Managing these conditions involves multiple medical fields, with Ophthalmology playing a pivotal role. As a Maxillofacial Surgeon, my responsibilities include performing biopsies, tumour removal, orbital decompression, and orbital and eyelid reconstruction.
Orbital tumours and inflammatory diseases do not have specific symptoms. They may manifest as proptosis (eye bulging), eye redness, eye pain, visual impairment, diplopia (double vision), eyelid ptosis, epiphora (constant tearing), headaches or nasal obstruction.
Imaging techniques such as CT scans and MRIs are crucial for evaluation. While fine needle biopsy may provide a faster and more cost-effective means of obtaining a diagnosis and differentiating between benign and malignant orbital masses, a definitive diagnosis often requires an open biopsy, especially for bone, neural tumours, and lymphomas.
The most common types of orbital tumours include:
- Vascular malformations: are benign tumours that frequently involve the orbital tissues. Surgery can be a solution when the lesion causes symptoms. In specific cases, interventional (neuro)radiology may help in vascular diagnostic angiography or therapeutic vascular embolization.
- Mesenchymal tumours: this category encompasses a wide variety of usually benign tumours, such as lipomas. Solitary fibrous tumours within this group are locally aggressive and require removal, although distant metastases are rare.
- Schwannoma or neurilemmomas are benign tumours that originate from neural cells. Asymptomatic cases should be monitored regularly, but surgical intervention is necessary for gliomas and meningiomas, often in collaboration with Neurosurgery.
- Tumours originating from the orbital bone: Benign symptomatic tumours are surgically removed while preserving the eye structure. Malignant cases require prompt and radical excision.
- Lymphoma, particularly MALT lymphomas, are not uncommon and require a biopsy for confirmation. Treatment is managed by a Hematologist using appropriate drugs.
- Eyelid and facial skin tumours can invade the orbit and should be surgically removed. A new drug (vismodegib) enlarges the treatment options for selected patients with unresectable or potentially eye-threatening basal cell carcinoma. Still, its prescription must be approved and directed by an oncology board. Radiotherapy is a valid option for certain orbital-invading skin tumours.
- Lesions originating from thelacrimal sac and nasal sinus can also invade the orbit and should be referred to a surgeon.
- Lacrimal gland tumours: Although rare, these tumours must also be surgically removed.
Inflammatory diseases
Inflammatory orbital diseases can be classified into two main categories:
- Non-specific or idiopathic: Previously known as inflammatory pseudotumor, this condition mimics the clinical presentation of an orbital tumour. A biopsy is essential, but even experienced pathologists may find it challenging to differentiate from lymphoma. Exploring underlying causes may reveal IgG4 immune-mediated syndromes or other rheumatological diseases, such as sarcoidosis or lupus, requiring consultation with autoimmune disease specialists.
- Graves’ disease: This autoimmune disease, which causes thyroid hyperfunction, has a specific association with the orbit and eyes, known as Graves’ orbitopathy or thyroid eye disease. It is classified into three severity categories: mild, moderate, and sight-threatening. Even in mild and moderate cases, it significantly impacts the quality of life.
Graves’ disease
Graves’ disease involves abnormal thyroid function due to an autoimmune response. Approximately 25% to 30% of individuals with Graves’ disease develop Graves’ orbitopathy, characterized by inflammatory changes in the orbit and eyes. The disease severity ranges from mild and moderate to sight-threatening, with negative impacts on quality of life even in mild and moderate cases.
In Graves’ orbitopathy, there is an abnormal growth of adipose (fat) and muscle tissues within the non-distensible bony cavity of the orbit. This growth leads to proptosis (eye bulging), eyelid retraction, and an inability to close the eyelids properly, resulting in corneal dryness and potential corneal ulcers. Additionally, it can alter light refraction and optical power and increase the risk of severe eye infections.
Muscle dysfunction and misalignment of the eyes may cause double vision. Compression of the optic nerve by the surrounding tissues can lead to vision loss and requires urgent medical and surgical intervention.
Patients with Graves’ disease may also experience other symptoms of hyperthyroidism, such as tachycardia, excessive sweating, diarrhoea, and an enlarged neck.
General recommendations
The first and most essential action patients can take is to quit smoking and adopt a healthy lifestyle to reduce cholesterol levels.
Optimal control of thyroid hormones is crucial. Eye ointments with artificial tears and gels alleviate dry eye symptoms. Therefore, prompt consultation with an Endocrinologist and an Ophthalmologist is essential.
Depending on the disease activity and severity, the multidisciplinary medical team may recommend corticosteroid treatment, immunomodulatory drugs, or, in selected cases, radiotherapy.
In sight-threatening Graves’ orbitopathy that does not respond adequately to medication, prompt referral to a surgeon is necessary for orbital decompression to relieve pressure on the optic nerve. Endoscopic approaches through the nose can treat mild cases. Severe ones may require a skin incision to access the lateral (external) orbital wall.
For inactive or stable disease, rehabilitative surgery may include eyelid surgery and orbital decompression.
If you suspect you have Graves’ disease or an orbital tumour, don’t hesitate to contact us for a comprehensive multidisciplinary evaluation.