Intro
Temporomandibular joint. Know more about its anatomy, dysfunction symptoms and signs and treatment strategies conservative (dental care, mouthguards, exercices,…) and interventional treatments.
The temporomandibular joints: the joints we use the most
They move approximately 2000x per day.
We need them for the survival functions of eating and drinking, but they are essential for speaking and for producing many of the
facial expressions that convey human feelings and emotions.
It s not surprising that temporomandibular disorders, otherwise known as temporomandibular dysfunction, is a very common condition.
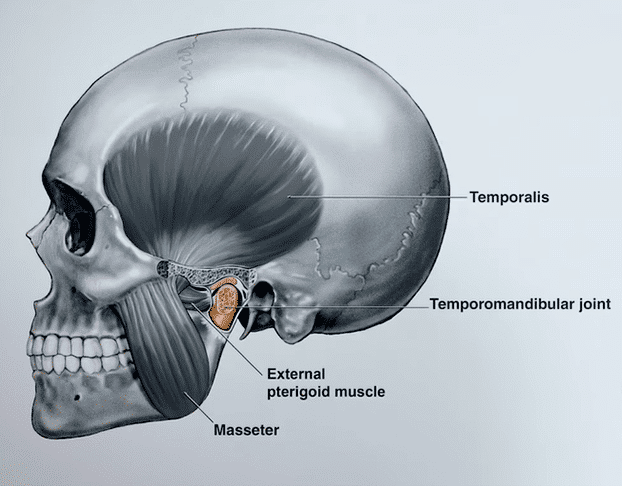
Anatomy
Both joints are composed of a: mandibular condyle, a bone sphere that fits in a fossa of the temporal bone.
Between the bone surfaces, there is an articular disc. This disc is supported by ligaments posteriorly and anteriorly is it attached to a muscle (lateral pterigoid muscle).
The joints have natural lubricant called synovial fluid. All these structures are encased by a fibrous capsule.
During function, the condyle rotates and slides forward and downward, and together with the disc, they leave the fossa, and move under a bone eminence. This movement requires a complex coordination of an extensive muscle system.
Symptoms and Signs
The three major symptoms and signs of temporomandibular dysfunction are:
pain, functional impairment and joint sounds.
As far as pain is concerned, it may arise either from the joint or the masticatory muscles.
It may irradiate to other facial locations, in particular to the ear, because the joint lies so closely to it. So, the first perception of pain might not give you a direct clue to the actual source of the pain. Actually, temporomandibular dysfunction is also know as Costen syndrome, named after James Costen (1895-1962), an American Otolaryngologist who first published on this orofacial pain.
There can be changes in the range and direction of the jaw movement (functional imparment). This must be divided into two categories:
Limitations of the jaw movement, because of a mechanical blockade stopping the movement, or just as a self-restriction to avoid pain.
Alternatively, there can also be a joint luxation, when there is an excessive movement.
Another common complaint is the annoyance caused by joint sounds. The most common noise is the clicking sound caused by non-synchronous movements of the disc and the condyle or a crepitation sound when the bone surfaces of the mandibula and temporal rub onto each other, in the case of degenerative joint disease.
Translating signs and symptoms into a diagnosis
These symptoms and signs that we have just seen, are the basic guidelines to pointing to a diagnosis, within the extensive list
of the diagnostic chart.
Actually, temporomandibular dysfunction is not a diagnostic term on its own. It is rather an umbrella term, for a set of approximately thirty health disorders. However, the term temporomandibular disorders is generally used to refer to the subset of the most frequent conditions within the list shown in the video (3:27).
It should be noted that, temporomandibular disorders can range from a single isolated condition to multi-system involvement, which
means that diagnostic chart can be expanded even further. For many patients, in particular those with chronic symptoms, there might be an overlap with other health conditions, such as headaches, bruxism, sleep apnea, postural problems and psychological and psychiatric disorders, namely: anxiety and depression.
Prevalence
Temporomandibular disorders are highly prevalent.
But for most it will be a mild and transient condition. However symptoms may persist chronically with high impact in the quality of life. TMD associated chronic pain is the third most common chronic pain condition after headaches and lower back pain.
Temporomandibular disorders are twice as prevalent in women than in men.
Symptomatic variability
The reasons behind this gender difference and, in fact the causes of temporomandibular disorders, are still under a long on-going investigation. It is believed to be a combination of different factors, here I will mention only a few of them:
mechanical instability (for example when there are missing teeth),
different hormonal sensitivity,
different inflammatory reactions,
different pain sensitivity and modulation.
The different levels on how these factors play in each of us, may explain one of the most intriguing characteristics of temporomandibular disorders: a huge symptomatic variability.
Imaging and symptoms not often correlate
The magnetic resonance images show a dislocated disc (video 5:04). They could belong to any hypothetical patients, but the symptomatic
expression would range from no symptoms at all, to an occasional joint movement disorder or a long-lasting pain with severe interference in the quality of life.
Despite having similar imaging features the need for care and treatment strategies are different between them.
Treatment
Treatment strategies are driven mainly by the symptoms of each patient.
But since there a wide range of different symptomatic expressions and intensities, and an extensive diagnostic list, as you have seen, there isn’t a care pathway for temporomandibular disorders, because one size does not fit all.
Instead, every treatment plan must be tailored.
One very important point in all treatment plans is education. Explaining to the patient their condition is the main pillar for effective
self-management, particularly in patients with chronic pain.
In general, it’s possible to organize treatment plans as: conservative or interventional.
Conservative treatments
In the conservative therapies:
A very important starting point is to restore missing teeth, to provide stability to the joints, to restore full masticatory capacity, correct phonetics and overall facial aesthetics.
Medication is used to reduce joint inflammation, short term or long-term pain relief and muscle relaxation
Intra oral appliances (mouthguards) are a very frequently prescribed treatment. There are dozens of designs, but in my opinion, the one you are seeing now (Michigan splint / Michigan mouthguard) is the most effective in providing good stability and pressure relief.
General exercise is beneficial for your overall health and to correct postural imbalances, which is also key for a correct normal head and neck muscle function. You can also do specific jaw exercises on your own, but always according to the status of your joint health. Do not stress your joint if in acute pain or when suffering from other acute symptoms. Take time to rest and only start moving the joint slowly, with controlled movements, restoring the muscular strength, as you would do for any other ill joint.
Physical therapy, might be a solution when in need of an expert in rehabilitation assistance.
Interventional treatments
The interventional procedures list includes:
Arthrocentesis, which means to flush inflammatory mediators from the joint and to release joint adhesions through hydraulic pressure. It may provide a way to inject medication inside the joint.
Arthroscopy uses a very small camera inside the joint, for a visual diagnosis of its interior and together with other instruments, it is possible to performminimal invasive surgical procedures
These two procedures tend to have a very quick recovery time and are almost scarless.
Open surgery remains an important component of temporomandibular disorders care, for properly selected patients, such as: recurrent luxations, joint replacement for a prothesis in severely damaged joints, traumatic and tumoral cases, as well as selected cases that did not respond to previous approaches.
A successful treatment plan for temporomandibular disorders must address possible co-morbidities, and therefore call on-board an intertwined network of other professionals, such as rheumatologists, neurologists, physical therapists or chronic pain clinicians, providing a global care, coordinated by a health professional that looks to into the whole spectrum of diagnostic chart and is able to integrate the full portfolio of therapeutic.
Advanced reading
My reference authors on temporomandibular dysfunction are: Daniele Manfredini, Florencio Monje, Dorit Nitzan, Eric Schiffman among other.
From a vast literature on temporomandibular dysfunction, I also recommend the following papers:
Bond E. et al, Committee on Temporomandibular Disorders (TMDs): From Research Discoveries to Clinical Treatment
Schiffman E. et al., Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group
Meurechy N. et al, Postoperative Physiotherapy After Open Temporomandibular Joint Surgery: A 3-Step Program
Extras
Know more about the biography of James Costen (click here).
Some celebrities of the showbiz industry have allegedly been diagnosed with temporomandibular dysfunction:
– Iggy Azalea
– LeAnn Rimes
– Burt Reynolds
The movie Poison Ivy, from 1992, has a brief reference to the symptoms of temporomandibular dysfunction, including the Burt Reynolds torments.